Osteoarthritis of the knee joint means a decrease in the performance of cartilage due to its curvature and destruction. Other terms are used to denote this disease -gonarthrosisanddeforming osteoarthritis. Several methods are currently used to treat the disease: a specific option is chosen taking into account the individual characteristics of the patient.
Specifics of the disease
Osteoarthritis of the knee usually develops progressively. It usually occurs in women and the elderly with overweight or venous defects. The disease can occur on one or both knees at once.
The main stages of development of osteoarthritis of the knee:
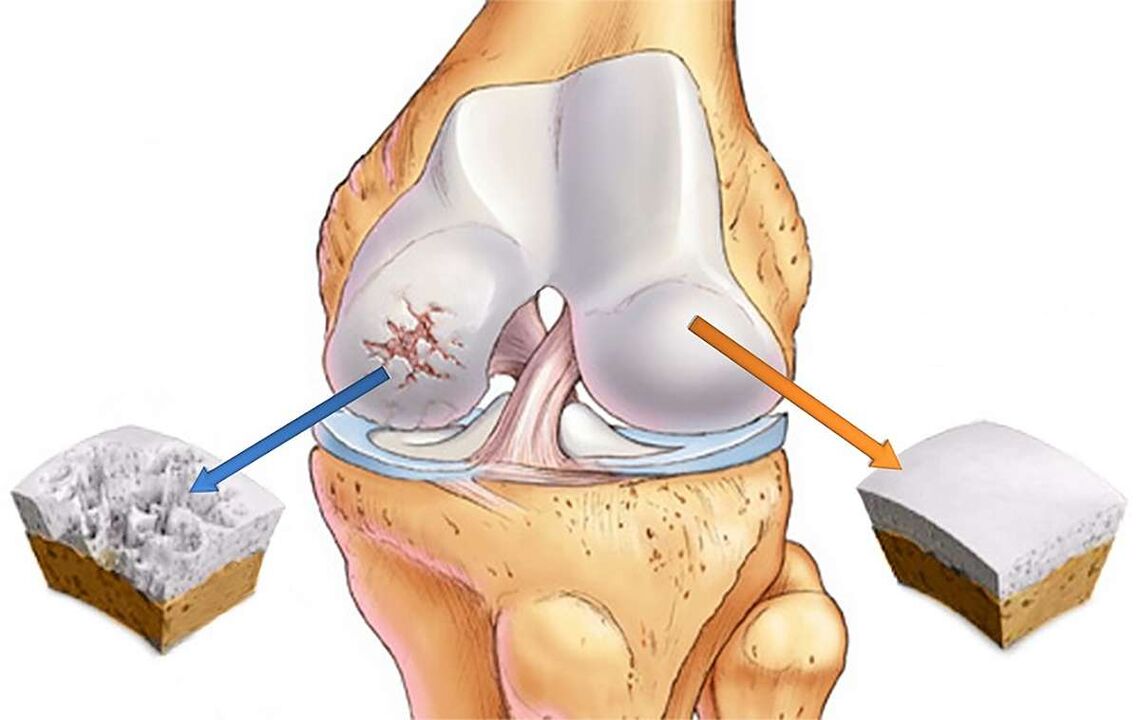
- Initially. There is a decrease in the amortization parameters of the joint due to the mutual friction of the cartilage and an increase in their roughness. Cracking is sometimes observed.
- Second. At this stage, the bone begins to be covered with growths (osteophytes). A curvature is fixed on the inner surface of the joint bag, stiffness in the work of the limb is observed. As a result, the knee joint gradually reduces its functionality. Due to the reduction in the thickness of the intercartilaginous membrane, a reduction in the distance between the tibia and the femur is observed.
- Third. If nothing is done, the pain in the knee area becomes permanent due to irreversible damage to the cartilage tissue. At this stage, the patient can no longer move normally.
The first symptoms of osteoarthritis of the knee are sufficient reason to consult a specialist. Otherwise there is a real danger of becoming disabled.

Why osteoarthritis occurs
The main reasons for the development of osteoarthritis of the knee:
- hereditary predisposition;
- temporary immobility of the knee joint as a result of injury;
- surgical removal of the meniscus;
- high physical activity, constant hypothermia;
- obesity, overweight problems;
- breaking ties (weakening them);
- other joint diseases (arthritis, swelling, various inflammations);
- disorders of normal metabolism, calcium deficiency in the body;
- flat feet (failure of the center of gravity increases the pressure on the joint);
- stress, general fatigue, lack of sleep.
Symptoms
Signs of possible osteoarthritis of the knee:
- Pain in the knee joint. The pain appears suddenly, against the background of physical exertion. In the first stage we talk about almost imperceptible lumbago, later the disease becomes more serious.
- Visual violation of the shape of the knee. This happens in the later stages.
- Accumulation of fluid, Baker's cyst. These are tangible seals in the back of the knee joint.
- The appearance of cartilage on cartilage, against the background of sharp pain. This indicates the second or third stage of gonarthrosis.
- Inflammation of the inside of the joint bag. Manifested by swelling and enlargement of cartilage.
- Knee stiffness due to severe pain, to complete immobilization. This happens in the advanced stages of the disease.
Treatment
Effective treatment of osteoarthritis of the knee is possible only with the use of an integrated approach. Modern medicine still can not offer any specific drug to eliminate this disorder. The success of treatment procedures depends on the timeliness of detection of the problem, which allows you to start the fight against gonarthrosis in the early stages.
Starting treatment, the specialist pursues several goals:
- reduce the symptoms of pain as much as possible;
- to restore the normal flow of nutrients to the joint;
- increase the intensity of blood circulation in the knee area;
- restoring the functionality of the supporting muscles in the problem area;
- make the knee as mobile as possible;
- widening the space between the connected bones.
The exact treatment algorithm is determined individually. Distinguish between conservative and surgical techniques.
conservative method
This approach is used in the early stages of the disease and is the use of various drugs and therapeutic exercises.
Painkillers, anti-inflammatory drugs
To eliminate or reduce pain in the knee joint, the doctor usually prescribes the use of non-steroidal anti-inflammatory drugs. In pharmacies they are represented by tablets, ointments and injections. Warming and anesthetic gels, ointments and patches have shown good efficacy in relieving pain.
A positive result in this case is usually achieved in 3-4 days. It should be understood that these drugs do not eliminate the disease, but only reduce the pain. It is recommended to take painkillers only on the advice of a specialist and only when fixing unbearable pain. The fact is that NSAIDs provoke the appearance of various side effects (especially suffering from the gastrointestinal tract).
Hormonal drugs
In some cases, your doctor may prescribe hormonal injections to relieve the pain of osteoarthritis of the knee. This approach is used when the effectiveness of NSAIDs is weak against the background of progressive disease.
Hormones are prescribed for a short period (1-10 days) during the exacerbation of osteoarthritis and accumulation of fluid in the knee joint.
Chondroprotectors
To restore and nourish the cartilage layer at the beginning of the disease, the so-called chondroprotectors (glucosamine, chondroitin sulfate). Glucosamine starts the process of cartilage regeneration, corrects metabolism, blocks destructive processes. Chondroitin sulfate disarms dangerous enzymes, increases the amount of collagen (this protein nourishes cartilage with moisture). According to leading doctors, these drugs currently show the greatest positive effect in the treatment of gonarthrosis.
In particularly critical cases, when the cartilage tissue has suffered serious abnormalities, chondroprotectors are ineffective. When prescribing glucosamine and chondroin sulfate, the doctor indicates specific daily doses. Only a systematic approach to taking these drugs gives a chance for positive results. On sale they are represented by tablets, capsules, injections, gels.
Vasodilators
To eliminate spasms of the vascular system, optimize blood flow and metabolism in the knee, the doctor prescribes vasodilators. As a rule, they are prescribed in combination with chondroprotectors. If against the background of osteoarthritis the fluid in the knee does not collect, it is allowed to rub the joint with a warming ointment and to attend sessions for therapeutic massage.
Hyaluronic acid
In its chemical composition, this substance is very close to the intra-articular fluid. Once introduced into the joint, the acid generates a film that protects the cartilage from rubbing against each other. It is allowed to use the drug after stopping the exacerbation.
Therapeutic gymnastics
For osteoarthritis of the knee,resort to exercise therapy, but only under strict supervision of your doctor or experienced coach. Self-medication is strictly forbidden, given the huge risks of any careless movements and loads. Proper use of physiotherapy exercises helps keep the joint in working order, eliminates muscle spasms and relieves unpleasant symptoms. It is strictly forbidden to engage in physiotherapy exercises during exacerbations or in inappropriate conditions.
Physiotherapy
With proper application of physiotherapy techniques, you can significantly reduce knee pain, relieve inflammation and improve the flow of nutrients to joint tissue. Before prescribing physiotherapy, the orthopedist conducts a detailed diagnosis of the problem area, prescribes general and special tests, sends an ultrasound or X-ray. This approach allows you to draw a real picture of the problem and choose the best methods.
The following types of physiotherapy have a good analgesic effect:
- UV radiation. Due to exposure to ultraviolet rays, there is a decrease in the sensitivity of nerve endings and a reduction in pain. It is usually prescribed in the later stages of the disease. The standard duration of treatment is 7-8 sessions.
- Local magnetic therapy. Improves the overall health of the patient by reducing pain, inflammation, muscle spasms. Magnetic therapy is usually prescribed at the first fixation of the symptoms of osteoarthritis of the knee. The standard number of procedures is 20-25 sessions of 30 minutes each.
- Infrared laser therapy, UHF, SMW devices, ultrasound, therapeutic baths, etc.
If the disease has passed into a stage of dystrophic and deforming changes, the doctor recommends spa treatment. After careful study of the patient's history, a specific list of procedures is compiled.

Surgery
This approach, when properly applied, is able to partially or completely restore the work of the knee joint. The formation of the algorithm for surgical intervention takes into account the level of destruction of cartilage tissue, the degree of inflammation, the amount of fluid collected, etc. As a rule, surgical intervention is practiced in the late stages of gonarthrosis. This approach involves fragmentary or complete replacement of the affected joint with an endoprosthesis.
The main approaches to surgical treatment:
- Arthrodesis of the joint. During the operation, the surgeon fixes the legs in the most comfortable position for the patient, followed by immobilization of the knee joint. Defective cartilage is completely eliminated. Such a radical approach is only appropriate in extreme cases.
- Arthroscopic debridement. It is used in the second stage of development of osteoarthritis of the knee joint. Surgical removal of damaged cartilage tissue is performed, which allows you to save a person from pain for several years (usually 2-3 years).
- Endoprosthesis. In this case, the knee joint or its individual part is replaced with a plastic, ceramic or metal implant, which completely repeats the anatomical configuration of the natural joint. Endoprosthesis is today considered the most effective way to restore a full life to a knee suffering from osteoarthritis for the next 15-20 years.
Competent planning and conduct of surgical treatment makes it possible to improve the patient's well-being and restore his mobility (partially or completely). At the same time, it should be understood that after the operation you will need a long period of recovery, attending physiotherapy exercises, mechanotherapy, diet and more.
Rehabilitation
On average, the rehabilitation period after surgery takes 90 days:
The main tasks of rehabilitation:
- restoring the patient's ability to move normally;
- optimizing the functioning of muscles and joints;
- creating a protective block for the prosthesis.
The drainage is removed 2-3 days after the operation, after which you can try to walk carefully. To relieve pain, the doctor prescribes drugs with a cooling effect. The small symptoms of pain sometimes last for a year after the operation: this is due to the fact that the prosthesis needs time to heal. Elderly patients recover longer: NSAIDs are prescribed to alleviate their condition. In some situations, the doctor prescribes hormonal drugs that have a pronounced effect.
One week later, the patient entered the rehabilitation center under the care of an experienced physiotherapist. When developing a course of training therapy, the individual characteristics of the body are taken into account. Classes are held regularly (daily), with a gradual increase in load: this protects against injuries and tears of tissues.
Period after discharge
At the end of the stay in the rehabilitation center, the patient is discharged and given detailed recommendations about his future lifestyle. Dancing and light gymnastics are allowed after 6 months from the date of surgery. As for serious loads (running, jumping, sports, heavy squats), they must be completely excluded. Otherwise the prosthesis will fail quickly.
Do not lift heavy objects weighing more than 25 kg. Supporting railings need to be installed inside the apartment: they are placed on the stairs, in the shower and the bathroom. All furniture must be fully functional (especially chairs). These and other measures will maximize the life of the prosthesis. You should also be prepared for postoperative osteoarthritis of the knee, which can last up to 3 years.
Prevention of the disease
The best way to deal with any disease is to prevent it from occurring.
Effective waysprevention of osteoarthritis of the knee:
- Proper nutrition, maintaining a normal weight. It is better to eliminate from your diet fatty and fried foods, alcohol, coffee, etc. An experienced nutritionist can give detailed advice on this.
- Be careful when exercising. It is desirable to minimize the load on the joints.
- Be careful of any diseases (especially infectious), treat them properly and avoid chronic stages.
- Be careful of your posture, do not be careless about diseases of the bones and spine.
- Include light physical activity in your daily routine (cycling, swimming, walking, doing strengthening exercises for the joints).
- Avoid any self-medication for knee arthritis. At the first symptoms of the disease you should contact the clinic immediately.
- Lead a quiet lifestyle without stress and lack of sleep.
- Take measures to strengthen immunity (hardening, intake of vitamins).
- Dress warmly during the cold season.
By applying the principles of a healthy lifestyle in your life and seek medical help in a timely manner, you can minimize the risks of developing osteoarthritis of the knee joints. When choosing a clinic, preference should be given to proven treatment centers equipped with modern equipment.



















